For plan details and complete lists of the commercial plans offered, see:
- 2026 Summary of Companies, Lines of Business, Networks, and Benefit Plans.
- 2025 Summary of Companies, Lines of Business, Networks, and Benefit Plans.
The summaries linked above indicate which benefit plans are part of a network or line of business covered by your ConnectiCare contract.
To easily determine if you or a provider you work for is in-network for a ConnectiCare member, use the Check Provider Network Status tool in the Member Management section of the provider portal.
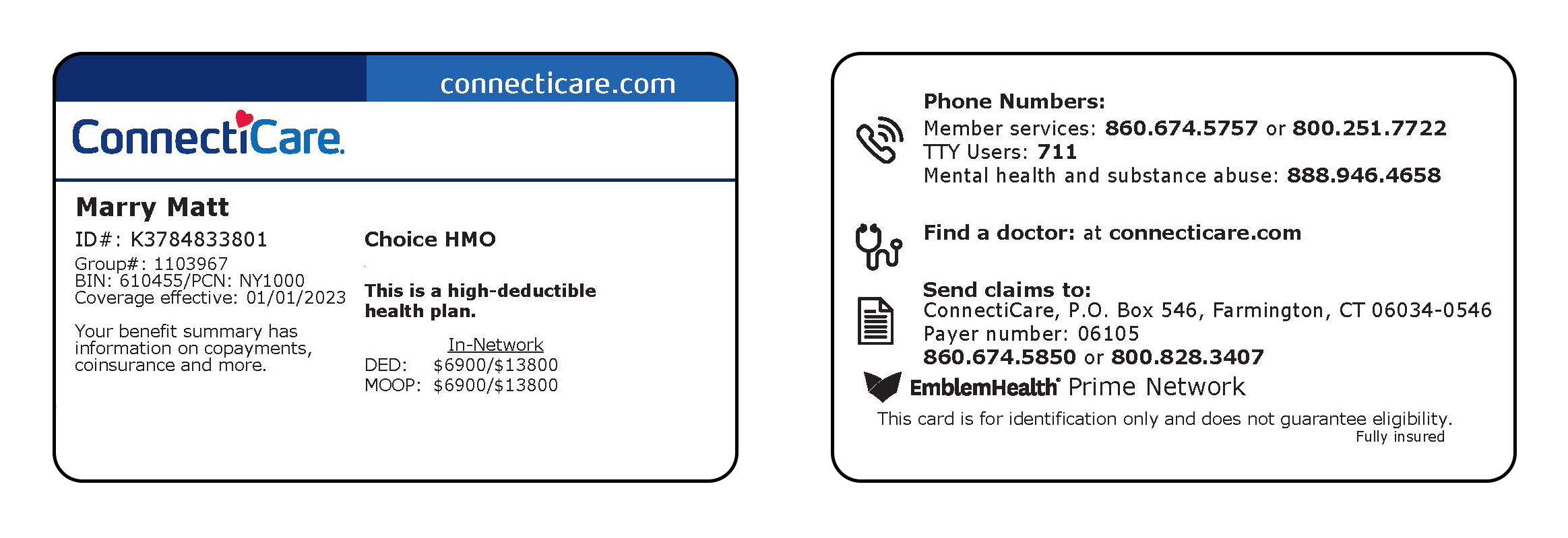
Choice Network
The benefit plans that use the Choice Network let members manage their health their way. They may use any of the doctors, hospitals, labs, and facilities in our large network covering Connecticut.
Members do not need a PCP and do not need referrals to see specialists in this network.