Medicare Networks and Benefit Plans
Resources To Help You Care for Our Medicare Members.
Please encourage interested patients to view our Medicare Advantage plans.
Please encourage interested patients to view our Medicare Advantage plans.
Plan benefits and cost-sharing change every year. See Drugs Covered by Medicare Plans. One of the big changes brings is the lower out-of-pocket costs for members with prescription drug coverage. The new threshold is $2,000, after which all covered prescription drugs will be available at $0 copay.
For a list of ConnectiCare’s Medicare plans and their corresponding networks, along with details including member cost-shares, service areas, and referral requirements, see:
The summaries linked above indicate which benefit plans are part of a network or line of business covered by your ConnectiCare contract. To easily determine if you are in-network for a ConnectiCare Medicare member, use the Availity Essentials provider portal.
Choice Network
The benefit plans that use the Choice Network let Medicare members manage their health their way. They may use any of the doctors, hospitals, labs, and facilities in our large network covering Connecticut. Members do not need a primary care provider (PCP) and do not need referrals to see specialists in this network.
Passage Network
The benefit plans that use the Passage Network require Medicare members to designate a PCP to coordinate their care. Members do not need referrals to see specialists in this network.
Medicare members have an ID number that may begin with “K” or an all-numeric ID number with 13 digits that begins with “8”. For these members, providers should follow ConnectiCare’s new operational changes as outlined in the provider hub, beginning Jan. 1, 2026.
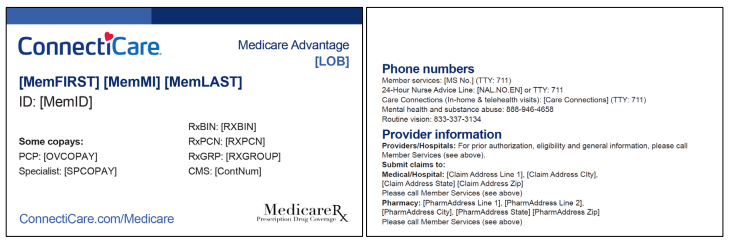
The following is a sample Medicare member ID card. Please note:
To review the list of covered prescription drugs for Medicare members, see the 2026 Medicare Formulary.
For helpful resources in coordinating care for Medicare members, see Clinical Information, Coverage Guidelines, Medical Coverage Criteria, and the health care services chapter of the 2026 Medicare Provider Manual.
The Quality Improvement webpage also offers resources, including the Comprehensive CAHPS Guide and Tips to Improve Member Satisfaction
Please encourage your patients to complete the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) if they are selected for the survey sample.
Care Management for Special Needs Plan Members
To review the requirements for providers involved in the care of dual-eligible special needs plan (D-SNP) members, see the health care services chapter of the 2026 Medicare Provider Manual.
Medicare and special needs plan members will receive a call from ConnectiCare asking them to complete a health risk assessment (HRA). Please encourage your patients to complete this survey. This will help our care management team better address members' needs and direct them to appropriate care and support services.
In 2026, we will continue to offer the ConnectiCare -Medicare Member Rewards Program to encourage Medicare members to receive primary care and key health screenings. Please reach out to your patients to schedule these important preventive exams.
Medicare members may be eligible for rewards when completing their HRA within the first 90 days of enrollment. D-SNP members may also be eligible for rewards when completing an annual HRA.
Our Medicare members will have continued support from Medicare Connect Concierge in 2026. This is the one phone number members can call when they need help solving their health care needs. Medicare Connect Concierge can help:
To reach Medicare Connect Concierge, please call 800-224-2273 (TTY: 711). From Oct. 1 to March 31, you can call us seven days a week from 8 a.m. to 8 p.m. From April 1 to Sept. 30, you can call us Monday through Friday from 8 a.m. to 8 p.m.
For helpful resources regarding claims for Medicare members, see the claims chapter of the 2026 Medicare Provider Manual.
Contracted time frames in provider agreements will supersede time frames in this guide if your provider agreement provides for a longer time period.
Clinic Visit Policy
If you provide our Medicare Advantage members with hospital-owned and operated clinic visit services, please review our clinic visit policy and correct coding requirements. ConnectiCare will monitor compliance with this policy and may recoup payment from providers for non complaince.
Reminder: For services rendered in place of service (POS) 19, off-campus hospital-owned locations, claims billed with the G0463 clinic code should include the Modifier PO.
Members who are fully dual-eligible for Medicare and Medicaid and classified as Qualified Medicare Beneficiaries (QMB) should not be held liable for Medicare Part A and B cost sharing when the state or another payor is responsible for paying such amounts. Providers are responsible for verifying eligibility and obtaining approval for those services that require prior authorization.
Providers agree that under no circumstance shall a member be liable to the provider for any sums that are the legal obligation of ConnectiCare to the provider. Balance billing a member for covered services is prohibited, except for the member’s applicable copayment, coinsurance, and deductible amounts.
For helpful resources regarding claim dispute/appeal, see the claims chapter of the 2026 Medicare Provider Manual. Contracted time frames in provider agreements will supersede time frames in this guide to the extent that your provider agreement provides for more time.
ConnectiCare expects its contracted providers to prevent and address fraud, waste, and abuse. To learn about this important topic, see the compliance chapter of the 2026 Medicare Provider Manual.
ConnectiCare offers educational opportunities in culturally and linguistically appropriate practices and concepts for providers and their staff. Web-based training modules are available on the Availity Essentials provider portal.
The NOTICE Act requires all hospitals, including critical access hospitals, to provide the Medicare Outpatient Observation Notice (MOON) to Medicare beneficiaries, including Medicare Advantage enrollees, who receive observation services as an outpatient for more than 24 hours. For more information, see the health care services chapter of the 2026 Medicare Provider Manual.