ConnectiCare offers affordable health plans both on and off the Connecticut Exchange.
For a list of these Marketplace plans and their corresponding networks, along with details including member cost-shares, service areas, and referral requirements, see:- 2026 Summary of Companies, Lines of Business, Networks, and Benefit Plans.
- 2025 Summary of Companies, Lines of Business, Networks, and Benefit Plans.
The summaries linked above indicate which benefit plans are part of a network or line of business covered by your ConnectiCare contract.
To easily determine if you are in-network for a ConnectiCare Marketplace member, use the Availity Essentials provider portal.
Value Network
ConnectiCare has a tailored network called Value that is offered to individual members who purchase health benefit plans from ConnectiCare Insurance Company, Inc. through Access Health CT.
Our Value Network features a tailored network that is a subset of our Choice Network. It may be the right solution for individuals who can choose care options within a more localized area.
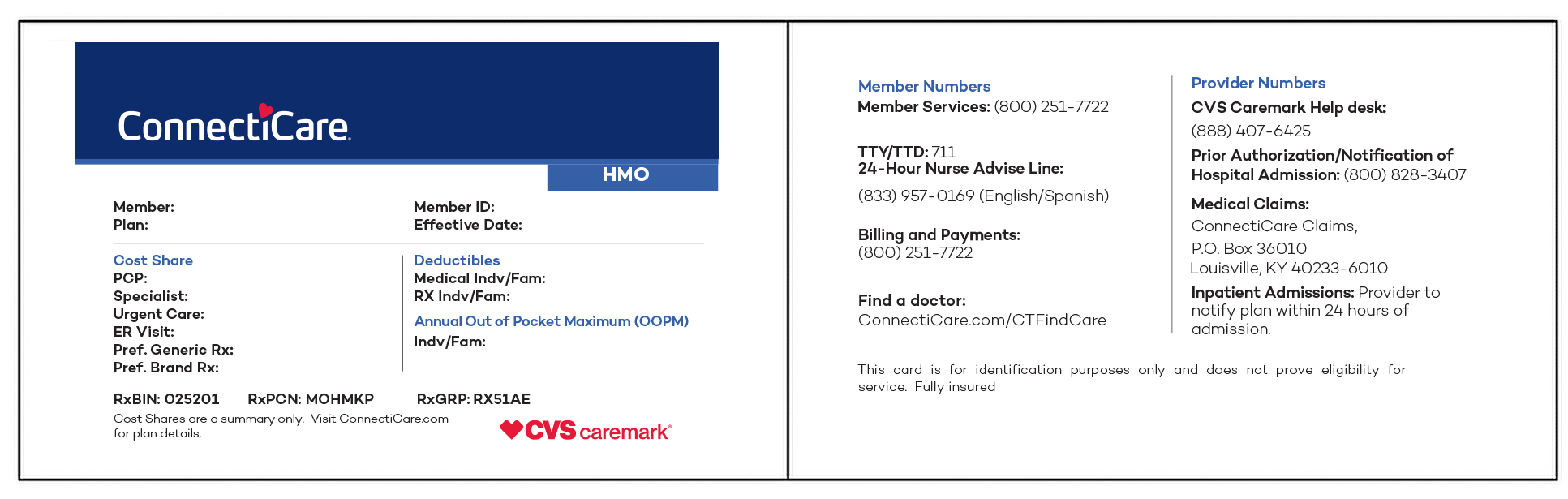
ConnectiCare member ID cards will clearly indicate whether a member has selected the Value Network. Members do not need a primary care provider (PCP) and do not need referrals to see specialists in this network.
Choice Network
The benefit plans that use the Choice Network let members manage their health their way. They may use any of the doctors, hospitals, labs, and facilities in our large network covering Connecticut.
Members do not need a PCP and do not need referrals to see specialists in this network.
Plans Retired in 2026
The Choice EPO, Choice POS, and Value EPO plans for Marketplace members are being retired and will not be available in 2026.